Information about facial nerve palsy
- Facial palsy is a devastating condition for the patient and their family
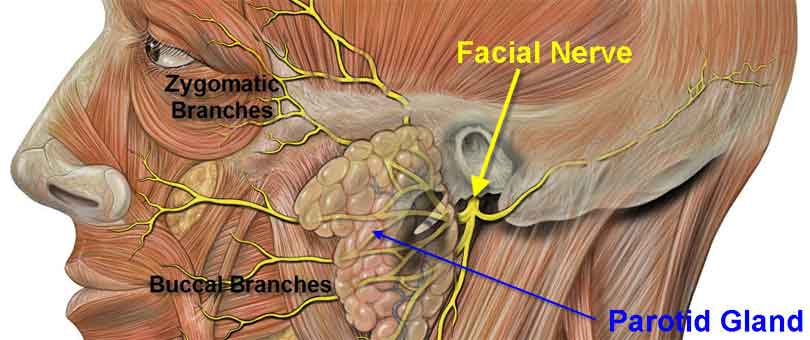
- Facial nerve palsy may occur spontaneously following trauma or surgical procedure or as a result of malignant tumours of the ear, parotid gland or skull base
- Paralysis that involves all divisions of the facial nerve is peripheral, while paralysis sparing the forehead is central
- Facial palsy is usually graded on a scale of 1 to 6 where 1 is normal and 6 is complete paralysis
Bell’s palsy
- Bell’s palsy is a unilateral facial nerve paralysis that is by definition idiopathic
- Studies have demonstrated that herpetic infection may be responsible so a better term might be viral or herpetic facial paralysis
- The clinical course of Bell’s palsy is characteristic:
- The onset is sudden with the patient often noticing the symptoms upon waking from sleep
- The recovery is gradual but spontaneous recovery can be expected in more than 85% of cases
- Medical therapy within three days with oral steroids and antiviral medication has been shown to decrease the incidence of incomplete recovery
Facial palsy symptoms
- Gradual onset of symptoms (over months), paralysis that doesn’t begin to recover after several months or recurrent symptoms on the same side suggest tumour and should be further evaluated by an ENT specialist
- Studies have shown that up to 30% of patients diagnosed with idiopathic Bell’s palsy were found to have another cause for their facial paralysis such as a facial nerve neuroma, parotid gland malignancy or cerebello-pontine angle tumour
Ramsay-Hunt Syndrome
- Ramsay-Hunt syndrome or herpes zoster oticus is another syndrome that includes facial nerve paralysis
- Symptoms include facial paralysis together with severe pain and a vesicular eruption in the external auditory canal and auricle in the distribution of the facial nerve
- The vesicular lesions generally precede the facial nerve paralysis but this isn’t always the case
- Vesicles may be non-painful, small or even undetectable
- The prognosis for recovery is significantly poorer than in Bell’s palsy
- Medical therapy with antiviral agents and oral steroids is standard and should be started as early as the diagnosis is made
Temporal bone fractures
- The facial nerve has an elongated course throughout the temporal bone
- Significant trauma producing a temporal bone fracture can involve the facial nerve either by direct transection or oedema and conduction block
- Unless the facial nerve has been completely transacted the swelling and facial neuropraxia can take up to 72 hours to develop – so careful assessment of the facial nerve at the initial presentation is important in later management decisions
- Unfortunately in this situation the patient has usually suffered significant head trauma and may have multiple injuries – with facial nerve assessment not an immediate priority
- CT scanning of the petrous temporal bone can be done to assess the facial nerve along its intratemporal course – if the nerve appears to be impaled by a bony spicule or transection management by an ENT specialist is indicated
- Temporal bone trauma can also affect the hearing and balance
- If the fracture involves the middle ear or ear canal then conductive hearing loss may occur secondary to a haemotympanum, discontinuity of the ossicular chain or ear drum perforation
Eye care in facial palsy
- The facial nerve provides a critical function to the eye – namely eye closure
- Eye closure provides a valuable protective function of maintaining moisture to the cornea
- The eyelid blink sweeps tears over the cornea and eyelid closure at night prevents the cornea from drying
- Without this protection the cornea can become progressively more dry causing significant pain, corneal ulceration, scarring and ultimately permanent changes in vision
- Also the eyelid blink reflex protects the eye by preventing foreign bodies from contacting the surface and damaging the cornea
- Patients with facial paralysis need to use artificial tears frequently during the day as well as a moisture lubricant at night while they sleep
- A clear plastic moisture chamber for protection and humidification may also be helpful to prevent eye drying during sleep
- The best treatment for corneal injuries is prevention by meticulous eye care
- Surgical rehabilitation is possible with placement of a gold weight into the upper eyelid – this may give an almost natural appearance and functional result