The salivary glands
- The major salivary glands are the parotid glands, submandibular glands and sublingual glands
- There are also a large number (600-1,000) of minor salivary glands widely distributed throughout the oral mucosa, palate, uvula, floor of the mouth, posterior tongue, retromolar and peritonsillar area, pharynx, larynx and paranasal sinuses
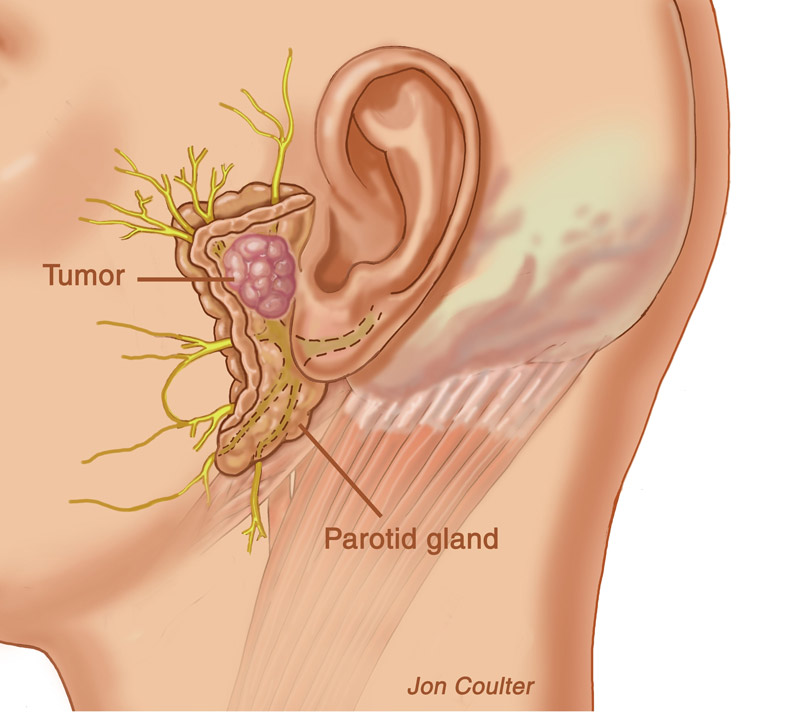
- Tumours affecting salivary glands may be benign or malignant and are diverse in their pathology
- 80% of salivary gland tumours arise in the parotid glands, 10-15% in the submandibular glands and the remainder in the sublingual and minor salivary glands
- About 80% of parotid neoplasms are benign but the relative proportion of malignancy increases in smaller glands
- About half of submandibular gland neoplasms and most sublingual and minor salivary gland tumours are malignant
Salivary gland tumours
- Neoplasms of salivary glands have an incidence of about 1 to 2 per 100,000
- They are fewer than 1% of all cancers and 3-6% of all tumours of the head and neck
- Tumours are most common in the 6th decade of life
- Malignancy typically presents after age 60, whilst benign lesions usually occur after age 40
- Benign tumours are more common in women, but malignant tumours have an equal sex distribution
- Certain ethnic groups, e.g. Inuit populations, have a higher rate of salivary gland tumours which is maintained even after migration to a low incidence area
- The responsible environmental or genetic factors are unknown
Types of salivary gland tumours
- Benign (non-cancerous) tumours
- Pleomorphic adenoma (most common)
- Also called benign mixed tumour, is the most common tumour of the parotid gland and causes over a third of submandibular tumours
- They are slow-growing and asymptomatic
- Warthin’s tumour
- Rarities including oncocytomas and monomorphic adenomas
- In children, most parotid tumours are benign and are haemangiomas
Salivary gland cancer
The malignant tumours most commonly affecting the major salivary glands are mucoepidermoid carcinoma, acinic cell carcinoma and adenoid cystic carcinomas
Among the minor salivary glands, adenoid cystic carcinoma is the most common
Malignant tumours are designated high-grade or low-grade dependent on their histology
High-grade:
- Mucoepidermoid carcinoma (grade III)
- Mucoepidermoid carcinoma is the most common malignancy of the parotid gland and is the second most common of the submandibular gland (after adenoid cystic carcinoma)
- It represents about 8% of all parotid tumours
- Adenocarcinoma – poorly differentiated carcinoma and anaplastic carcinoma; represents 2-3% of salivary tumours
- Squamous cell carcinoma
- Malignant mixed tumours
- Adenoid cystic carcinoma
Low-grade:
- Acinic cell tumours: represent 1% of all salivary gland neoplasms and 95% arise in the parotid gland
- Mucoepidermoid carcinoma (grades I or II)
- Regional metastases from skin or mucosal malignancies may present as salivary gland masses
- 1-3% of patients with cutaneous squamous cell carcinoma (SCC) of the head and neck experience metastatic spread to the parotid-area lymph nodes
- Lymphomas may occasionally present in a salivary gland
Salivary gland cancer staging
- Staging is most commonly based on the tumour, node and metastasis (TNM) classification system – based on tumour size, spread to cervical lymph node and distant metastases
- It correlates with survival and assists treatment decisions
Risk factors for salivary gland tumours
- Radiation to the neck increases the risk of malignancy of salivary glands with a 15- to 20-year latency
- Smoking is an important risk factor for the development of Warthin’s tumours but its relationship to malignant parotid tumours is less clear
- Warthin’s tumours are eight times more common in smokers compared with non-smokers
- Some studies have suggested an association between high use of mobile phones and an increased risk of benign and malignant parotid tumours – although others have found no evidence of such a relationship
Salivary gland tumour symptoms
- Most salivary gland neoplasms are a slowly enlarging painless mass
- Parotid neoplasms most commonly occur in the tail of the gland as a discrete mass in an otherwise normal gland
- Submandibular neoplasms often appear with diffuse enlargement of the gland
- Sublingual tumours produce a palpable fullness in the floor of the mouth
- Minor salivary gland tumours vary according on the site of origin – painless masses on the palate or floor of the mouth are the most common form but laryngeal salivary gland tumours can produce airway obstruction, dysphagia, or hoarseness
- Facial palsy with a salivary gland mass indicates malignancy
- Pain can occur with both benign and malignant tumours
- Pain may arise from suppuration or haemorrhage into a mass or from infiltration of adjacent tissue
- In the nasal cavity or paranasal sinus they cause nasal obstruction or sinusitis
Salivary gland tumour signs
Use bimanual palpation of the lateral pharyngeal wall for deep lobe parotid tumours and the extent of submandibular and sublingual masses
Clinical features of a salivary gland mass suggestive of malignancy are:
- Hardness
- Fixation
- Tenderness
- Infiltration of surrounding structures, e.g. facial nerve, local lymph nodes
- Overlying skin ulceration
- Cranial nerve palsy
- History of head and neck SCC or melanoma
Salivary gland investigations
Imaging to define location, detect malignant features, assess local extension and invasion, and detect metastases and systemic involvement
Ultrasound
- Ultrasound is the usual initial means to assess superficial lesions
- Ultrasound is more limited at visualising the deep lobe of the parotid and some minor salivary glands depending on location
- Ultrasound-guided fine needle aspiration (FNA) cytology is used to obtain cytological confirmation. CT-guided biopsy can also be used
CT and MRI scanning
- If deep tissue extension is suspected or malignancy confirmed on cytology, an MRI or CT scan is used to evaluate tumour bulk, local invasion and perineural spread
- CT is better for bony imaging and MRI better defines soft tissue characteristics
- All tumours in the sublingual gland should be imaged with MRI as the risk of malignancy is high
- For lesions of the deep lobe of parotid gland and the minor salivary glands, MRI and CT scanning are the imaging methods of choice
Sialography
- Sialography can be used to delineate the salivary ductal system and is useful for patients with a suspected salivary sinus or fistula
Management of salivary gland tumours
- Most current treatment depends on surgical ablation of the tumour
- Radiotherapy may be used following surgery, usually for higher-grade tumours, or alone for non-resectable tumours – its use improves overall survival in high-grade, advanced parotid cancer as an adjunct to surgery
- Response of malignant tumours to single-agent chemotherapy is generally poor and tends to be reserved for the palliative management of advanced disease that is not amenable to local therapies such as surgery and/or radiation
- Polychemotherapy is likely to induce a higher response rate, but has not been shown to improve survival
- Targeted molecular therapy is hoped to bring breakthroughs
Surgery for salivary gland tumours
Parotid tumours
- Superficial parotidectomy with careful dissection of the facial nerve is required for diagnosis and treatment of a parotid mass
- For malignant parotid tumours, a more radical procedure sacrificing the facial nerve may be necessary, depending on the extent of infiltration – reconstruction using free tissue transfer will be needed in this situation
Submandibular gland tumours
- Benign neoplasms of the submandibular gland require complete excision of the gland
Click here for more information about parotid and submandibular gland surgery
Minor salivary gland tumours
- Up to 60% of patients with malignant minor salivary gland tumours of the larynx will develop recurrent disease locally, regionally, or at distant sites
- Because of the high risk of recurrence, total laryngectomy is usually recommended for patients with minor salivary gland cancer
Complications
Facial nerve
- Damage to the facial nerve may occur as a result of parotid tumour infiltration or surgery
- Risk of damage is higher with repeat operations and facial nerve monitoring may reduce this risk
Recurrence of benign or malignant tumours
- Pleomorphic adenomas must be completely removed at primary surgery as recurrent tumours are often multifocal and can occur 10-15 years later with much reduced cure rates (<25%)
Malignant change
- Pleomorphic adenomas can undergo malignant change and are called carcinoma ex-pleomorphic adenoma
- They represent about 2-4% of salivary gland malignancies
- Sudden rapid growth of a previously stable mass is typical
- They are aggressive and have a poor prognosis
Frey’s syndrome
- Redness and sweating on the cheek, which can appear when eating, seeing or thinking about certain kinds of food which produce strong salivation) can occur after parotid surgery
- The autonomic nerves reform inappropriately (parasympathetic impulses going to sympathetic nerves) so that a stimulus to salivation will make the face sweat
Xerostomia and oral mucositis
- This may occur following radiotherapy
Follow-up after salivary gland surgery
- Follow-up of patients who have had parotidectomy for benign or malignant disease shows remarkably little adverse effect on the quality of life
Prognosis
- Because salivary gland tumours are rare and so diverse, there is a shortage of good clinical trials
- It is hoped that a better understanding of their molecular biology will lead to improved understanding of prognosis and better treatment
- The mean 5-year survival for advanced high-grade parotid cancer is 35% and where there is facial nerve involvement, this falls to 9%
- Earlier-stage disease has a better prognosis – 10-year survival for stage I parotid tumours (tumour <2 cm with no local or metastatic spread) is 83%
- Tumours in children and adolescents are sometimes malignant but the prognosis tends to be good
Indications for referral to an ENT – head and neck surgeon
- When there is an unexplained lump in the neck, of recent onset, or a previously undiagnosed lump that has changed over a period of 3-6 weeks
- There is an unexplained persistent swelling in the parotid or submandibular gland
- The patient has an unexplained persistent sore or painful throat
- There has been unilateral unexplained pain in the head and neck area for more than 4 weeks, associated with otalgia but a normal otoscopy
- There has been unexplained ulceration of the oral mucosa or mass persisting for more than 3 weeks
- There are unexplained red and white patches of the oral mucosa that are painful or swollen or bleeding
- There have been persistent symptoms or signs related to the oral cavity (>6 weeks) and a definitive diagnosis of a benign lesion cannot be made