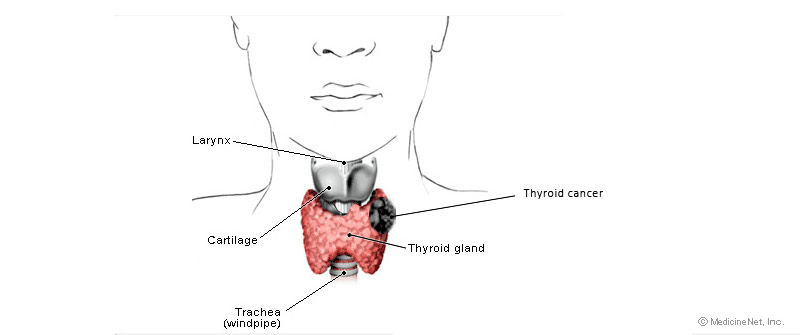
Thyroid cancer information
- Many more women than men have thyroid nodules – however, a thyroid nodule in a male has a higher risk of being cancerous than a nodule in a female
- Thyroid nodules in patients with normal thyroid function require fine needle biopsy which provides specific information about the nature of the nodule – patients with atypical fine needle biopsy have up to a 20% risk of malignancy and require appropriate thyroid surgery
- The key issue for patients with thyroid nodules is whether surgery is required to remove the nodule for accurate diagnosis by pathology
- Older people are more likely to develop thyroid nodules – however, a nodule in a person younger than 40 years of age has a higher chance of being cancerous than a nodule in a person over 40
- People who receive irradiation as children are also at increased risk of developing thyroid cancer
Thyroid cancer symptoms
Some of the symptoms that may point to thyroid cancer include:
- A lump, or nodule in the neck — especially in the front of the neck, in the area of the Adam’s apple
- Enlargement of the neck
- Enlarged of neck lymph glands
- Hoarseness, difficulty speaking normally, voice changes
- Difficulty swallowing (dysphagia), or a choking feeling
- Difficulty breathing
- Pain in the neck or throat, including pain from the neck to the ears
- Sensitivity in the neck — discomfort with neckties, turtlenecks, scarves, necklaces
- Persistent or chronic cough not due to allergies or illness
- Asymmetry in the thyroid (big nodule on one side, nothing on the other)
- Nodules that when manipulated give the impression that the entire thyroid is moving
Types of thyroid cancer
The four major types of thyroid cancer listed in increasing order of aggressiveness are:
- Papillary
- Follicular (including the Hürthle cell variant)
- Medullary
- Anaplastic
Papillary thyroid cancer
- Approximately 80% of thyroid cancers are papillary
- Papillary thyroid cancers may have a follicular component, but any amount of papillary disease means the tumour will behave like a papillary tumour
- These tumours can be multifocal in the thyroid gland and often spread to the neck lymph nodes
- The presence of neck lymph nodes doesn’t appear to affect survival rates
- Papillary cancer factors which indicate a better prognosis include:
- Size smaller than 1.5cm
- The absence of thyroid gland capsule involvement
- Papillary thyroid cancer often follow an indolent course when discovered in people under age 30-40
- Therefore people diagnosed with papillary thyroid cancer under age 30 ultimately may live longer
Papillary thyroid cancer treatment
- Total thyroidectomy when compared with subtotal, may significantly decrease the local recurrence rate (18% vs. 7%) and ultimately the mortality rate (1.5% to 0.03%)
- Treatment with radioactive iodine and thyroid hormone suppression decreases the incidence of recurrence from 11% to 3% compared with thyroid suppression alone
- If papillary thyroid cancer has spread to the neck nodes then a modified radical neck dissection is indicated
Follicular thyroid cancer
- Approximately 15% of thyroid cancer is follicular
- Two major types are microinvasive and macroinvasive
- The surgical specimen of all thyroid cancers must be sectioned completely to determine if the tumour capsule or any blood vessels are invaded – invasion can’t be seen on a fine needle aspirate and requires the whole specimen to be removed and submitted for pathology analysis
- Follicular thyroid carcinoma spreads by the blood stream
- A variant is called Hürthle cell carcinoma
Follicular thyroid cancer treatment
- Total thyroidectomy is considered the treatment of choice followed by post operative radioactive iodine and thyroid suppression
- Follicular carcinoma has a greater affinity for radioactive iodine compared with papillary carcinoma – therefore removal of all thyroid tissue allows a higher dose of I131 to be given
Medullary thyroid cancer
- Medullary carcinoma accounts for 6-10% of all thyroid cancer
- There are two forms: familial (20%) and sporadic (80%)
- Medullary carcinoma tends to involve both sides of the thyroid gland and the cell of origin is the parafollicular or C-cell
- Medullary carcinoma spreads to the neck nodes around 50% of the time
- The familial form is usually a component of multiple endocrine neoplasia (MEN) syndrome IIa and IIb
- MEN IIa is parathyroid adenoma, medullary thyroid carcinoma and pheochromocytoma
- MEN IIb doesn’t have the parathyroid component but includes a Marfanoid habitus and mucosal neuromas
- All patients with Medullary thyroid carcinoma should be tested for catecholamines –if positive the pheochromocytoma should be found and excised first
- All first degree relatives of patients with medullary thyroid carcinoma should be tested for a calcitonin level – also the RET-proto-oncogene test is positive in most patients and can be detected by a blood test
Medullary thyroid cancer treatment
- Total thyroidectomy with bilateral neck dissections are recommended
- In patients with a neck mass, a modified radical neck dissection that encompasses all the involved levels of disease should be removed
- In all patients with the familial form, the abnormal parathyroid glands should also be removed
- A total thyroidectomy is always indicated in patients with inherited medullary thyroid cancer
- Family members with positive tests (calcitonin / RET- proto-oncogene) require a prophylactic total thyroidectomy
- C-cells don’t take up radioactive iodine so this form of treatment can’t be used for patients with medullary thyroid cancer
Anaplastic carcinoma
- This is a rare thyroid tumour with a poor prognosis
- The surgeon’s role is often limited to diagnosis and securing the airway
- These tumours are not usually resectable and are often treated with chemoradiotherapy for palliation
Thyroid lymphoma
- Thyroid lymphoma is included in the differential for anaplastic carcinoma because of the rapid growth, which often produces airway compromise
- Lymphomas often arise in patients with a history of Hashimoto’s thyoiditis, an autoimmune thyroid condition with lympocytic infiltration
- Rapid diagnosis and prompt therapy are necessary to prevent airway obstruction
Thyroid cancer summary
- An appreciation of the classification of thyroid cancer is important as there is a wide range of growth and behaviour
- At one end of the spectrum is papillary thyroid cancer which usually occurs in young adults, grows very slowly, spreads by lymph channels and is compatible with long life, even in the presence of spread
- At the other extreme is undifferentiated carcinoma which usually appears late in life and is invasive – most patients with anaplastic thyroid carcinoma succumb from local disease or pulmonary metastases or both
- Between the two extremes are follicular and medullary carcinomas, sarcomas, lymphomas and secondary tumours
- The cause of most cases of thyroid cancer is unknown although people who received low dose radiation to the head and neck have an increased risk of developing thyroid tumours
- The prognosis depends on many factors including the tumour type, the age of the patient and gender, and the local and regional tumour extent at the time of diagnosis
- The treatment of differentiated thyroid cancer is surgical removal
- Total thyroidectomy is recommended for papillary (>1.5cm), follicular, Hürtle cell and medullary carcinomas
- Appropriate neck dissection surgery is recommended to address lymph node involvement
- Following surgery patients with papillary or follicular thyroid cancer are usually treated with radioactive iodine to address potential residual disease
- All patients should be maintained on suppressive doses of thyroid hormone
- For patients with undifferentiated thyroid cancer the treatment usually requires a combination of surgery, chemotherapy and radiotherapy
Thyroid surgery by an ENT – head and neck surgeon
- ENT – head and neck surgeons can provide a complete evaluation and treatment options regarding thyroid problems
- An ENT specialist can receive up to 15 years of university and post-graduate training in surgery, concentrating on ear, nose and throat procedures
- Because they study the complex anatomy, physiology, and pathology of the entire head and neck, ENT specialists are uniquely qualified to perform the procedures that affect the thyroid gland